Abstract
BACKGROUND
Primary thrombocytosis (PT) that results from clonal bone marrow abnormality such as myeloproliferative neoplasm (MPN) can induce abnormal platelet function and acquired von Willebrand disease. Secondary thrombocytosis (ST) that may accompany inflammations, infections, malignancies, or stress is associated with elevated markers of the acute phase reactants, including C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR). The aim of this study is to evaluate role of platelet function tests by light transmission platelet aggregometry (LTA), plasma von Willebrand factor antigen (vWF:Ag), ristocetin cofactor activity (vWF:RCo) and inflammatory markers (ESR, CRP) for the differentiation of PT and ST.
METHODS
This was a prospective study in patients age 18 years or older with platelet counts higher than 450 x 109/L who admitted or attended the out-patient clinics in Chiang Mai University Hospital during November 2016 to June 2017. They were classified to PT from MPN according to WHO 2016 Classification and ST. Primary outcomes were sensitivity (Se) and specificity (Sp) of platelet function tests by LTA for the differentiation of PT and ST. Secondary outcomes were Se and Sp of ESR, CRP, vWF, and vWF:RCo for the differentiation of PT and ST as well as correlation between these markers and thrombohemorrhagic complications in patients with PT and ST. Categorical variables were compared using the Chi-squared test or Fisher exact test as appropriate. Continuous variables were compared by t-test or Wilcoxon rank-sum test (Mann-Whitney test). Level of significance was defined as p-value < 0.05.
RESULTS
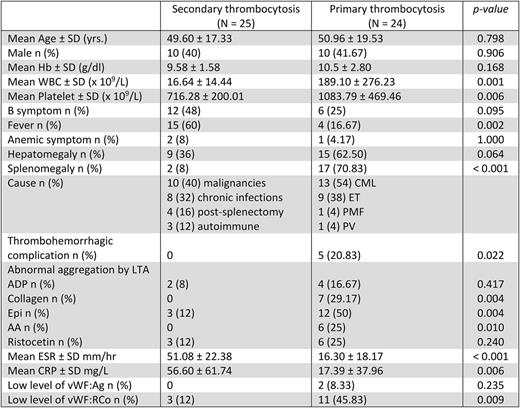
There were 49 patients enrolled in the study, mean age was 50.26 ± 18.26 years. Twenty-four patients (49%) had PT including 13 chronic myeloid leukemia (54%), 9 essential thrombocythemia (38%), 1 primary myelofibrosis (4%), and 1 polycythemia vera (4%). Twenty-five patients (51%) had ST including 10 malignancies (40%), 8 chronic infections (32%), 4 post-splenectomy (16%), and 3 autoimmune diseases (12%). Mean platelet count was higher in PT compared with ST (1083.79 ± 469.46 x 109/L and 716.28 ± 200.01 x 109/L respectively, p = 0.006). There was no difference in age and sex between groups. Abnormal LTA induced by collagen, arachidonic acid (AA), and epinephrine (Epi) were significantly presented in PT compared with ST (29%, 25%, and 50% respectively in PT; and 0%, 0%, 3% respectively in ST; p = 0.004, 0.010, and 0.004 respectively). The Se and Sp of collagen vs. AA vs. Epi-induced abnormal platelet aggregation for the differentiation of PT from ST were Se of 29.2% vs. 25% vs. 50%, and Sp of 100% vs. 100% vs. 88%, respectively. Mean ESR and CRP were significantly higher in ST (ESR 51.08 ± 22.38 mm/hr and CRP 56 ± 61.74 mg/L) compared with PT (ESR 16.30 ± 18.17 mm/hr and CRP 17.39 ± 37.96 mg/L; p < 0.001 and p = 0.006, respectively). The Se and Sp of ESR > 48 mm/hr in the differentiation of ST from PT were 76% and 91.7%, respectively while Se and Sp of CRP > 14.8 mg/L were 60% and 83.3%, respectively. No significant difference in proportion of patients with low vWF:Ag between groups (8.3% in PT and 0% in ST; p = 0.141) whereas PT group had significant higher proportion of patients with low vWF:RCo (45.8% in PT and 12.0% in ST; p = 0.009). The Se and Sp of abnormal vWF:RCo to differentiation of PT from ST were 45.8% and 88%, respectively. Thrombohemorrhagic complications at the time of diagnosis was 21% in PT while no complication in ST (p = 0.006). Risk factors of thrombohemorrhagic complications were platelet counts more than 1,569.8 x 109/L (p = 0.03) and Epi-induced abnormal platelet aggregometry (p = 0.02).
CONCLUSION
Abnormal platelet function determined by LTA with collagen, AA, epinephrine had high specificity to differentiate between PT and ST. vWF:RCo, ESR and CRP levels might be helpful for the differentiation of PT and ST. PT has higher incidence of thrombohemorrhagic complication compare to ST and is correlated with high platelet counts and Epi-induced abnormal platelet aggregometry.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal